Suicide Prevention

Suicide is the second leading cause of death for 15-34 year olds.
College students may be at a high risk for suicide due to the pressures of college life and the changes in environment. According to the CDC, approximately 1,100 college students die by suicide each year.
Compiled here are resources relating to suicide prevention best practices and research to aid campuses in providing effective suicide prevention.
For more information about campus campaigns, specifically Ask. Listen. Refer, please contact Margo Leitschuh at muwrcasklistenrefer@missouri.edu or (573) 882-9335
Scope
Quick Links
National Data | Missouri Data | Risk and Protective Factors | Warning Signs | Population ConsiderationsNational Data
Suicide is the second leading cause of death among 15-34 year olds.
For every person who dies by suicide, more than 30 others attempt suicide.
Among undergraduates and graduates from 2012, 7.1-7.7% of students seriously considered suicide, 2.3% made a plan, and .6-1.2% attempted suicide. The rates for individuals of the same age but not enrolled in college full time are all 1-2% higher.
Missouri Data
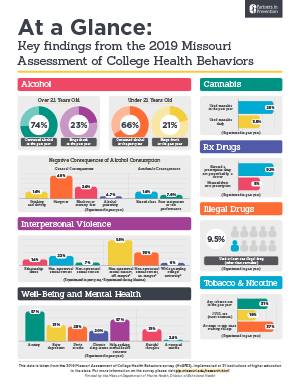
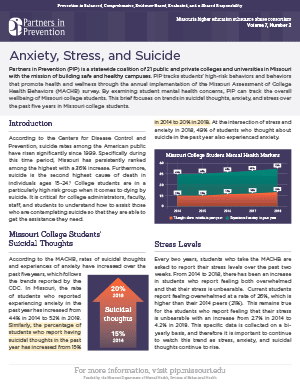
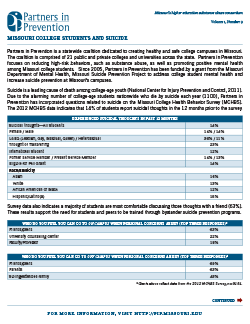
44% of Missouri college students report having suicidal thoughts at some point in their life and 23% report having suicidal thoughts in the past year
In the past year, 1.8% of Missouri college students report attempting suicide
58% of students who report having suicidal thoughts or who attempted suicide in the past year have not sought assistance
47% of students also report being concerned about a friend having suicidal thoughts or behaviors
Risk and Protective Factors
Risk Factors
Risk factors are characteristics that make it more likely that individuals will consider, attempt or die by suicide.
- Previous suicide attempts
- Mental Disorders, particularly depression, anxiety disorders, posttraumatic stress disorder, schizophrenia and certain personality disorders
- Alcohol or other substance use disorders
- Family history of mental disorder or substance use disorder
- History of trauma, abuse or sexual assault
- Family history of suicide or exposure to others that have died by suicide
- Family violence
- Chronic physical illness, including chronic pain
- Firearms in the home or access to other lethal means
- Lack of social support or social isolation
- Major life adjustment
- Incarceration
- Perfectionism
Protective Factors
The risk of suicide can be lowered by certain protective factors. They include:
- Having a support system (family, friends, and school)
- Spiritual Beliefs or participation in a religious community
- Good self-care and positive thinking
- Communication, planning, and problem-solving skills
- An ability to manage strong emotions
- Access to mental health care and willingness to accept help
- A school environment that encourages help seeking and promotes health
- Other environmental protections, such as reducing access to firearms and other lethal weapons
Warning Signs
Warning signs indicate an immediate possibility of suicide, whereas risk factors indicate someone has an increased likelihood for suicide, but indicate little or nothing about immediate danger.
- Starting or increasing use of alcohol or drugs
- Aggressive, impulsive, reckless or disruptive behavior
- Talking about death and dying, expressing a strong wish to die or talking about wanting “pain” to end
- Preoccupation with death
- Planning a suicide
- Giving away belongings, tying up loose ends, saying goodbye to friends and family
- Purchasing a firearm
- Obtaining other means of killing oneself
Population Considerations
Nearly 50% of U.S. military veteran college students reported considering suicide, and 20% reported currently having suicidal thoughts and a plan.5 An estimated 22 veterans die by suicide every day.
People who have experienced rape or sexual assault are 13 times more likely to attempt suicide than non-victims.
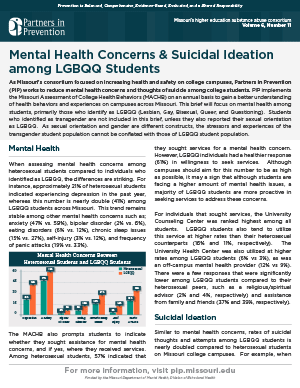
Lesbian, gay, bisexual, transgender, and questioning students are 3-4 times more likely to attempt suicide when compared to non-LGBTQ+ students.
Young adult American Indians and Alaskan Natives have higher rates of suicide deaths than young adults of any other ethnicity.
Asian-American students were more likely to have suicidal thoughts when compared with non-Asian-Americans.
Inside the African-American community, those ages 18-24 are most likely to think about and to attempt suicide.
Latino/a students are less likely to die by suicide, but those who were born in the U.S. report high levels of depression, suicidal thoughts, and attempts.
Overall, the completion rate for suicide is higher in men, especially European American/White men. This is because this group chooses more lethal means.
Data Briefs
Click on a brief below for more information.
At a Glance
Volume 8
Volume 7
Volume 6
Volume 5
Volume 4
Volume 3
Volume 2
Volume 1
Best Practices
Quick Links
Strategic Plan | Policies | Cultural Competencies | Interventions | Media ConsiderationsStrategic Plan
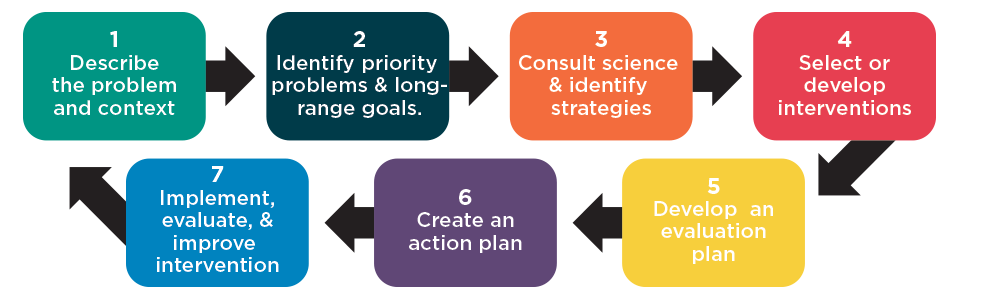
Identify a strategic plan to address suicide prevention. Keep in mind – what specific results or changes do you hope to achieve and how will those help reduce suicide?
Strategic Planning Process
Thomas Joiner's Model of Suicide Risk, 2006
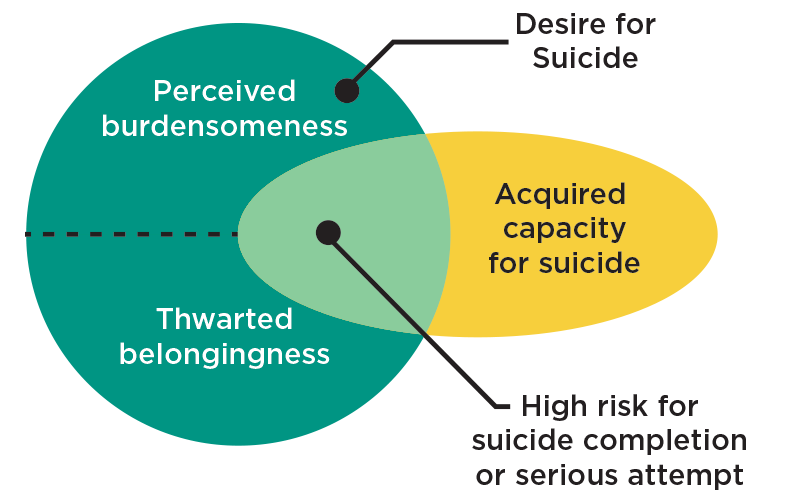
Wanting death is composed of two psychological experiences:
- A perception of being a burden to others (perceived burdensomeness). “I am worth more dead to the people that love me than I am alive.”
- Social disconnection to something larger than oneself (thwarted belongingness).
- By themselves, however, neither of these states is enough to move a person to act on the desire for death, but together with an acquired capacity (or fearlessness) they result in a high risk state for suicide.
- The risk is elevated where the two factors overlap – when a desire for suicide is met with the ability to carry it out.
What is acquired capacity?
- A series of painful and provocative experiences over the course of a lifetime can disinhibit a person from the fear of pain and death associated with suicide.
- Experiences may be trauma and abuse, high risk behaviors, injuries from contact sports, and a knowledge of and comfort with deadly means of suicide (e.g., firearms or lethal drugs).
- A previous suicide attempt is the strongest predictor of a future attempt.
Comprehensive Approach
- Shifting the paradigm from individual to problem-centered (Drum et al, 2009).
- Entire administrative structure of the university to become engaged with the problem of suicidality by intervening at all points along the suicidal continuum.
- Prevention, Early Intervention, Crisis Treatment, and Relapse PreventionM
- Expanding campus dialogue around issues of suicide to include all stakeholders will help involve a greater cross-section of campus personnel.
- Suicide Prevention Taskforce.
- Address policy issues on campus such as means restriction.
Suicide Prevention Resource Center
Please visit the Resources and Programs Page from the Suicide Prevention Resource Center for more about evidence-based practices (www.sprc.org/resources-programs)
After a Suicide: A Toolkit for Schools
www.sprc.org/resources-programs/after-suicide-toolkit-schools
National Action Alliance for Suicide Prevention
Visit the National Action Alliance for Suicide Prevention for resources and information regarding their strategy and work (actionallianceforsuicideprevention.org)
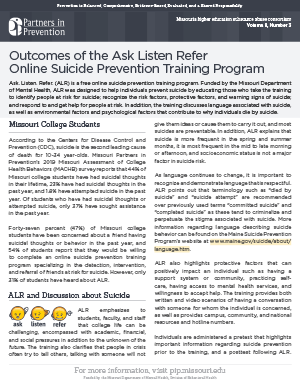
Ask. Listen. Refer
- Pretest (M=21.32, SD=3.46) and posttest (M=25.95, SD=3.57) scores measuring the consumer’s cultural knowledge of risk factors, warning signs, and protective factors of suicide indicated a statistically significant improvement from pretest to posttest (t=87.404, p< 0.000)
- In 2009, when the program began, early data analysis showed that 31.2% of consumers returned to the Ask Listen Refer site after their initial login. This suggests that the online training is appealing and consumers appreciate its constant availability.
Policies
The Show Me Compassionate Medical Education Act requires:
- Each public institution of higher education to develop and implement a policy to advise students and staff on suicide prevention programs available on and off campus that includes crisis intervention access, mental health program access, multimedia application access, student communication plans, and post intervention plans.
- Said policy should advise students, faculty, and staff for identifying and addressing the needs of students exhibiting suicidal tendencies or behaviors, and require training where appropriate.
- Institutions must provide all incoming students with information about depression and suicide prevention and must be available on the website of each institution.
- The Ask. Listen. Refer Training Program was designed to help faculty, staff, and students prevent suicide by teaching participants to identify people at risk for suicide; recognize the risk factors, protective factors and warning signs of suicide; and respond to and get help for people at risk. Ask. Listen. Refer is free for colleges and universities in the state of Missouri and includes a customized site with campus and community resources. We also provide a monthly newsletter with suicide prevention resources and data on who has completed the training on your campus. To view a demo site please visit asklistenrefer.org and click the link at the top of the page to view. For questions, concerns, or to get started with Ask. Listen. Refer for your campus please contact us at muwrcasklistenrefer@missouri.edu or at (573) 882-9335.
Cultural Competencies
The Suicide Prevention Resource Center has a great guide on creating linguistically and culturally competent suicide prevention materials and can be viewed here.
Cultural Risk and Protective Factors
Risk Factors:
- Among African Americans, anxiety is a bigger risk factor than depression or substance misuse.10 Also, the behavioralrisk factors of suicide, like those discussed on the previous screen, may be more pronounced in African Americans.
- The pressures of adjusting to an unfamiliar culture (called acculturative stress) is a risk factor common to many diverse groups, especially recent immigrants, including Asian students9 and Latinos.11 Acculturative barriers for international students can include homesickness and culture shock, language barriers, feeling isolated, less financial opportunity, experiences with prejudice and fear of seeking out mental health services.
- Mental health struggles, such as post-traumatic stress disorder (PTSD) and substance use, are common risk factors among returning veterans.
- Among students with mobility impairments and learning and emotional disabilities, all of the risk factors listed on the previous screen have been found to be more pronounced.15
- Asian and Asian American students are more likely to report physical symptoms than suicidal thoughts and emotions (depression, hopelessness, etc.). This relates to the cultural norm of not expressing feelings openly and a belief in the mind-body connection. They are also more susceptible to perfectionism as a risk factor.
- Since members of the LGBTQ+ community often experience higher rates of discrimination, harassment, and victimization, this can increase their rates of major depression, anxiety disorders, and substance use. This also greatly increases their risk factors for suicide. The number of attempted suicides is significantly higher for those who experience severe family rejection.
Protective Factors:
- Help-seeking behaviors and support networks can differ for different cultures.
- Social support and family harmony are important protective factors among Asian American students.
- Religiosity is a key protective factor for African American students. Friends, family, elders and other trusted community members are also key sources of support.
- Family support and family involvement in treatment is particularly important for Latino/a students, as the centrality of family, or familismo, is a core cultural value.
Interventions
Evidence-Based Interventions (taken from the Zero Suicide Toolkit: zerosuicide.sprc.org/toolkit/treat)
Evidence-based interventions include interventions and treatment that are designed to target suicide risk directly. These interventions have demonstrated effectiveness in reducing suicidal thoughts and behaviors.
At this time, only a few interventions are supported by research:
- Non-demand “caring contacts”
- Structured, problem-solving therapies
- Collaborative assessment and treatment planning1
Whichever specific model is used, interactions with patients should always be person-centered, collaborative, and careful to acknowledge the ambivalence that patients contemplating suicide risk often feel. Understanding that ambivalence—the desire to find a solution to the intense pain they feel versus the innate human desire to live—is essential for any clinician working with a patient at risk of suicide.
Non-Demand Caring Contacts
A growing body of evidence suggests that post-discharge follow-up contacts with high-risk individuals may be an effective suicide prevention strategy. While non-demand, caring contacts are not treatment per se, they can be used as adjuncts to treatment to:
- Keep patients engaged
- Follow up with patients who are difficult to engage
- Extend the connection between provider and patient after treatment has ended
Caring contact interventions include:
- Postcards and/or letters containing brief expressions of caring
- Telephone follow-up contacts with patients after discharge
- Telephone calls combined with in-person contact
- Organizations can use automated systems to send postcards, letters, e-mails, or text messages
Cognitive Behavioral Therapy for Suicide Prevention
This intervention, known as CBT-SP, is theoretically grounded in principles of cognitive behavior therapy (CBT); dialectical behavioral therapy (DBT); and targeted therapies for suicidal, depressed adolescents and adults.
Two studies tested the efficacy of this intervention: one study with adults, which found reductions in attempts and symptoms,, and a second study demonstrating the feasibility of using a similar intervention with adolescents.45 In Brown and colleagues' (2005) research with adults, a 10-session cognitive therapy intervention focused specifically on identifying proximal suicidal thoughts, images, and core beliefs activated before a suicide attempt. Subsequently, Stanley, Brown, and colleagues (2009) manualized a cognitive therapy intervention specifically for adolescent suicide attempters, called Cognitive Behavioral Therapy for Suicide Prevention (CBT-SP).
CBT-SP can be used with adults and adolescents and includes:
- Cognitive restructuring strategies, such as identifying and evaluating automatic thoughts from cognitive therapy
- Emotion regulation strategies, such as action urges and choices, emotions thermometer, index cue cards, mindfulness, opposite action, and distress tolerance skills from DBT
- Other CBT strategies, such as behavioral activation and problem-solving strategies5
- Because adolescents’ suicidal crises occur within an environment that may include problematic relationships, abuse, family dysfunction, or poor school performance, CBT-SP includes family interventions if needed
Dialectical Behavior Therapy (DBT)
The term dialectical means a synthesis or integration of opposites, and in DBT, it refers to the seemingly opposite strategies of acceptance and change.
DBT has four components, although these may be adjusted in practice to suit specific circumstances:
- A skills training group meeting once a week for 24 weeks
- Individual treatment once a week, running concurrently with the skills group
- Phone coaching, upon request by the client
- Consultation team meetings—a kind of “therapy for the therapists”6
- Numerous research studies, including several randomized control trials, have shown DBT to be effective in reducing suicidal behavior and other behavioral health issues. For example, Linehan et al. (2006) compared one year of DBT with women with borderline personality disorder and two or more suicide attempts and/or self-injuries in the past 5 years and at least one in the past 8 weeks to non-behavioral community treatment by experts. Those receiving DBT were significantly less likely to:
- Drop out of treatment
- Attempt suicide
- Visit psychiatric emergency rooms
- Experience psychiatric hospitalization
Collaborative Assessment and Management of Suicidality
Outpatient care is the explicit goal of the Collaborative Assessment and Management of Suicidality (CAMS), which is designed to strengthen the therapeutic alliance and increase patient motivation. CAMS is best understood as a therapeutic framework that emphasizes a collaborative assessment and treatment planning process between the patient at risk of suicide and the clinician. CAMS is supported by six published correlational studies and one randomized feasibility study, described briefly as follows:
- Two studies of suicidal college students in a college counseling center showed reductions in suicidal ideation.
- Two studies in outpatient settings in Denmark demonstrated the cross-cultural feasibility of CAMS.
- One study in an inpatient psychiatric setting showed reductions in suicidal ideation, depression, hopelessness, and suicidal cognitions.
- One study in U.S. Air Force outpatient clinics found suicidal ideation was reduced more quickly than in a control group. The intervention was also correlated with reductions in primary care appointments and emergency department visits.
- One study to test the feasibility of a randomized control trial, in an outpatient community mental health center, found reductions in suicidal ideation, overall symptom distress, and optimism/ hope, with the most robust effects occurring at the most distal assessment point—12 months after the start of treatment.8
Research-Informed Interventions
The standard of care for patients with suicide risk includes some interventions that may be informed by research and clinical practice but do not have a body of research to support them. Safety planning and lethal means reduction are two such interventions.
Safety Planning
A safety plan is a prioritized written list of coping strategies and sources of support developed by a clinician in collaboration with patients who are at high risk for suicide.9 According to Dr. Stanley's webinar presentation to the right, safety planning incorporates elements of four evidence-based suicide risk reduction strategies:
- Reducing access to lethal means
- Teaching brief problem-solving and coping skills
- Enhancing social support and identifying emergency contacts
- Using motivational enhancement to increase likelihood of engagement in further treatment
A safety plan is not a “no-suicide contract,” which is not recommended by experts in the field of suicide prevention. As they are generally used, no-suicide contracts ask patients to promise to stay alive without telling them how to stay alive.
Reducing Access to Lethal Means
Limiting access to medications and chemicals and removing or locking up firearms and other weapons are important actions to keep patients safe.10Reducing access to lethal means is based on the following suppositions:
- Many suicide attempts occur with little planning during a short-term crisis
- Intent isn’t all that determines whether an attempter lives or dies; means also matter
- 90% of attempters who survive do NOT go on to die by suicide later
- Access to firearms is a risk factor for suicide
- Firearms used in youth suicide usually belong to a parent
- Reducing access to lethal means saves lives
Reducing access to possible methods of suicide may be one of the most challenging tasks a clinician faces with a patient. Organization policies should clearly state what clinicians should do regarding lethal means, including the protocol to follow in the event a patient brings a weapon or other lethal means to the clinical setting.
Media Considerations
General Concerns and Recommendations regarding the Reporting of Suicide and Suicide Contagion
Suicide is often newsworthy, and it will probably be reported. The mission of a news organization is to report to the public information on events in the community. If a suicide is considered newsworthy, it will probably be reported. Health-care providers should realize that efforts to prevent news coverage may not be effective, and their goal should be to assist news professionals in their efforts toward responsible and accurate reporting.
"No Comment" is not a productive response to media representatives who are covering a suicide story. Refusing to speak with the media does not prevent coverage of suicide; rather, it precludes an opportunity to influence what will be contained in the report. Nevertheless, public officials should not feel obligated to provide an immediate answer to difficult questions. They should, however, be prepared to provide a reasonable timetable for giving such answers or be able to direct the media to someone who can provide the answers.
All parties should understand that a scientific basis exists for concern that news coverage of suicide may contribute to the causation of suicide. Efforts by persons trying to minimize suicide contagion are easily misinterpreted. Health officials must take the time to explain the carefully established, scientific basis for their concern about suicide contagion and how the potential for contagion can be reduced by responsible reporting.
Some characteristics of news coverage of suicide may contribute to contagion, and other characteristics may help prevent suicide. Clinicians and researchers acknowledge that it is not news coverage of suicide per se, but certain types of news coverage, that promote contagion. Persons concerned with preventing suicide contagion should be aware that certain characteristics of news coverage, rather than news coverage itself, should be avoided.
Health professionals or other public officials should not try to tell reporters what to report or how to write the news regarding suicide. If the nature and apparent mechanisms of suicide contagion are understood, the news media are more likely to present the news in a manner that minimizes the likelihood of such contagion. Instead of dictating what should be reported, public officials should explain the potential for suicide contagion, associated with certain types of reports and should suggest ways to minimize the risk for contagion.
Public officials and the news media should carefully consider what is to be said and reported regarding suicide. Reporters generally present the information that they are given. Impromptu comments about a suicide by a public official can result in harmful news coverage. Given the potential risks, public officials and the media should seek to minimize these risks by carefully considering what is to be said and reported regarding suicide.
Aspects of News Coverage That Can Promote Suicide Contagion
Presenting simplistic explanations for suicide. Suicide is never the result of a single factor or event, but rather results from a complex interaction of many factors and usually involves a history of psychosocial problems. Public officials and the media should carefully explain that the final precipitating event was not the only cause of a given suicide. Most persons who have completed suicide have had a history of problems that may not have been acknowledged during the acute aftermath of the suicide. Cataloguing the problems that could have played a causative role in a suicide is not necessary, but acknowledgement of these problems is recommended.
Engaging in repetitive, ongoing, or excessive reporting of suicide in the news. Repetitive and ongoing coverage, or prominent coverage, of a suicide tends to promote and maintain a preoccupation with suicide among at-risk persons, especially among persons 15-24 years of age. This preoccupation appears to be associated with suicide contagion. Information presented to the media should include the association between such coverage and the potential for suicide contagion. Public officials and media representatives should discuss alternative approaches for coverage of newsworthy suicide stories.
Providing sensational coverage of suicide. By its nature, news coverage of a suicidal event tends to heighten the general public's preoccupation with suicide. This reaction is also believed to be associated with contagion and the development of suicide clusters. Public officials can help minimize sensationalism by limiting, as much as possible, morbid details in their public discussions of suicide. News media professionals should attempt to decrease the prominence of the news report and avoid the use of dramatic photographs related to the suicide (e.g., photographs of the funeral, the deceased person's bedroom, and the site of the suicide).
Reporting "how-to" descriptions of suicide. Describing technical details about the method of suicide is undesirable. For example, reporting that a person died from carbon monoxide poisoning may not be harmful; however, providing details of the mechanisms and procedures used to complete the suicide may facilitate imitation of the suicidal behavior by other at-risk persons.
Presenting suicide as a tool for accomplishing certain ends. Suicide is usually a rare act of a troubled or depressed person. Presentation of suicide as a means of coping with personal problems (e.g., the break-up of a relationship or retaliation against parental discipline) may suggest suicide as a potential coping mechanism to at-risk persons. Although such factors often seem to trigger a suicidal act, other psychopathological problems are almost always involved. If suicide is presented as an effective means for ac-complishing specific ends, it may be perceived by a potentially suicidal person as an attractive solution.
Glorifying suicide or persons who complete suicide. News coverage is less likely to contribute to suicide contagion when reports of community expressions of grief (e.g. public eulogies, flying flags at half-mast, and erecting permanent public memorials) are minimized. Such actions may contribute to suicide contagion by suggesting to susceptible persons that society is honoring the suicidal behavior of the deceased person, rather than mourning the person's death.
Focusing on the suicide completer's positive characteristics. Empathy for family and friends often leads to a focus on reporting the positive aspects of a suicide completer's life. For example, friends or teachers may be quoted as saying the deceased person "was a great kid" or "had a bright future," and they avoid mentioning the troubles and problems that the deceased person experienced. As a result, statements venerating the deceased person are often reported in the news. However, if the suicide completer's problems are not acknowledged in the presence of these laudatory statements, suicidal behavior may appear attractive to other at-risk persons—especially those who rarely receive positive reinforcement for desirable behaviors.
National Resources
- Suicide Prevention Resource Center: sprc.org
- Zero Suicide in Health and Behavioral Health Care: zerosuicide.sprc.org
- National Action Alliance for Suicide Prevention: actionallianceforsuicideprevention.org
- Substance Abuse and Mental Health Services Administration (SAMHSA): samhsa.gov
- Missouri Institute of Mental Health (MIMH): mimh.edu
- National Alliance on Mental Illness (NAMI): nami.org
- National Suicide Prevention Lifeline: 1 (800) 273-8255
- Crisis Line: 1 (800) 833-3915
- Get Help Now: 1 (800) 999-9999
- LGBTQ Helpline: 1 (800) 488-7386
- Veterans’ Suicide Prevention Lifeline: 1 (800) 273-8255, then press 1
- Suicide Awareness and Prevention Among Asian Americans
- Suicide Text Lifeline: text “hello” to 741741
PIP Resources
Poster Campaigns
Poster Campaigns and Awareness Events Personalized for Each Campus
Real Stories: Addressing issues related to stigma of those who struggle with mental health issues or suicidal thoughts.
Connect: A program to encourage students to connect with resources and support systems on campus.
Ask. Listen. Refer
Free online suicide prevention program designed to help faculty, staff, and students prevent suicide by teaching them to:
- Identify people at risk for suicide
- Recognize the risk factors, protective factors, and warning signs of suicide among college students
- Respond to and get help for people at risk
Click here to access Ask Listen Refer!
Currently serves 41 campuses across the state of Missouri and 14 out of state schools. Visit asklistenrefer.org and click on your campus to take the training! To order promotional item for Ask. Listen. Refer, click here.
Research
Relevant Research Articles
- 2012 National Strategy for Suicide Prevention
- Suicide Trends Among Persons Aged 10–24 Years — United States, 1994–2012
- Suicide Among Racial/Ethnic Populations in the U.S. - Hispanics
- 12-Month and Lifetime Prevalence of Suicide Attempts Among Black Adolescents in the National Survey of American Life
- VA Suicide Prevention Program- Facts about Veteran Suicide. July 2016
- Suicide Among Asian- Americans
- LGBTQ and Mental Health
- Racial and Gender Disparities in Suicide Among Young Adults Aged 18–24: United States, 2009–2013
- Physical disability and suicidal ideation: a community-based study of risk/protective factors for suicidal thoughts
- Suicidal Thoughts among College Students More Common than Expected
Drum, D. J., Brownson, C., Burton Denmark, A., Smith, S. E. (2009). New data on the nature of suicidal crises in college students: Shifting the paradigm. Professional Psychology: Research and Practice, 40(3), 213-222.
Gallagher, R. P. (2004). National Survey of Counseling Center Directors. Arlington, VA: International Association of Counseling Services.
Westerfeld, J. S., Homaifar, B., Spotts, J., Furr, S., Range, L., &Werth, J. L. (2005). Perceptions concerning college student suicide: Data from four universities. Suicide and Life-Threatening Behavior, 35, 640-645.